High blood pressure is often dubbed the “silent killer”—and for good reason. Millions of people are walking around unaware that this silent force is gradually increasing their risk of heart attacks, strokes, kidney disease, and more. Traditionally, efforts to manage hypertension have focused almost exclusively on slashing sodium intake. While this strategy has some merit, recent nutritional science indicates we may be missing a crucial part of the puzzle: boosting potassium intake.
Potassium acts like a counterweight to sodium in the body. Where sodium raises blood pressure by causing the body to retain fluid, potassium helps the body excrete sodium and relax blood vessel walls, naturally reducing pressure. The challenge is that modern diets—rich in processed and fast foods—are sorely lacking in potassium. Dr. Lawrence Appel, a prominent researcher in cardiovascular health, notes, “The benefits of dietary potassium are as profound as those seen with many blood pressure medications.”
Understanding this balance shifts our paradigm. Instead of only focusing on what to cut out (sodium), we should also emphasize what to add in: potassium-rich foods like bananas, spinach, sweet potatoes, and beans. This blog post dives into why boosting potassium is just as important—if not more so—than cutting sodium, and offers a detailed, point-by-point exploration of strategies, science, and expert insight.

1- The Biological Balancing Act
Potassium and sodium function as electrolyte counterparts within our cellular structure. When we consume high levels of sodium without a corresponding intake of potassium, it leads to fluid retention, stiff arteries, and elevated blood pressure. Potassium helps regulate heartbeat, nerve function, and muscle contraction, all while ensuring the kidneys efficiently flush out excess sodium.
Studies from the Journal of the American Heart Association have shown that increasing dietary potassium significantly reduces systolic and diastolic blood pressure, especially in people consuming too much sodium. This symbiotic relationship isn’t just nutritional—it’s physiological. When potassium levels are adequate, the body finds its rhythm, and blood pressure is naturally moderated.

2- Shifting the Dietary Lens
Instead of obsessively avoiding salt shakers, it may be more impactful to look at what’s missing on our plates. The American diet is chronically deficient in potassium, often providing just half the daily recommended intake of 4,700 mg. Leafy greens, legumes, and starchy vegetables—key potassium sources—have been pushed aside for processed, salty fare.
Nutritionist and author Marion Nestle emphasizes that “eating real food—mostly plants—is the first and most effective step toward restoring mineral balance.” A high-potassium diet doesn’t require exotic ingredients or costly supplements; it begins with simple changes such as choosing a baked sweet potato over fries or adding spinach to your morning smoothie.

3- The DASH Diet and Potassium’s Role
The Dietary Approaches to Stop Hypertension (DASH) diet is rich in fruits, vegetables, whole grains, and low-fat dairy—all abundant in potassium. This eating pattern has long been lauded for its ability to lower blood pressure without the side effects of medication.
In The DASH Diet Action Plan by Marla Heller, the emphasis on potassium-rich foods is central. Research shows that following this diet can drop systolic blood pressure by 8–14 points—an effect comparable to pharmacological interventions. It’s not just about what’s eliminated, but what’s emphasized.

4- Fruits and Vegetables: Natural Potassium Powerhouses
Fresh produce is nature’s prescription for high blood pressure. Bananas, avocados, oranges, and beets are brimming with potassium and other heart-healthy nutrients. Including a colorful variety of fruits and vegetables daily ensures a steady supply of this essential mineral.
Dietary diversity is key. Tomatoes and potatoes, often overlooked, are among the highest potassium contributors in Western diets. As Michael Pollan suggests in In Defense of Food: “Eat food. Not too much. Mostly plants.” That’s a prescription not just for good health, but for balanced blood pressure as well.

5- Beans and Legumes: Affordable and Effective
Beans, lentils, and chickpeas are potassium-dense and highly accessible. One cup of cooked white beans, for example, delivers over 1,000 mg of potassium—nearly a quarter of your daily need.
Beyond their mineral content, legumes are high in fiber and protein, which further support cardiovascular health. According to Dr. Joel Fuhrman, “Legumes are an essential foundation of a longevity-promoting diet.” Affordable, versatile, and nutrient-packed, beans are an underutilized weapon in the battle against hypertension.

6- The Problem with Processed Foods
Processed foods are notoriously high in sodium and low in potassium, a double blow to blood pressure regulation. These convenient meals, snacks, and fast foods tip the mineral scale in sodium’s favor, leading to greater cardiovascular risk.
Consumer education is key. Learning to read nutrition labels and prioritizing whole foods over packaged ones can shift this imbalance. The New England Journal of Medicine found that reducing processed food consumption can lead to significant blood pressure reductions—without any other lifestyle changes.

7- Cultural and Economic Barriers
Accessibility and affordability often influence food choices more than nutrition knowledge. In many low-income communities, fresh produce and whole foods are harder to come by than packaged snacks and instant meals. This disparity reinforces poor mineral balance and health inequities.
Policymakers and public health advocates are beginning to recognize this. Subsidizing farmers’ markets, incentivizing healthy food outlets in food deserts, and expanding SNAP benefits for produce are practical strategies for closing the potassium gap.

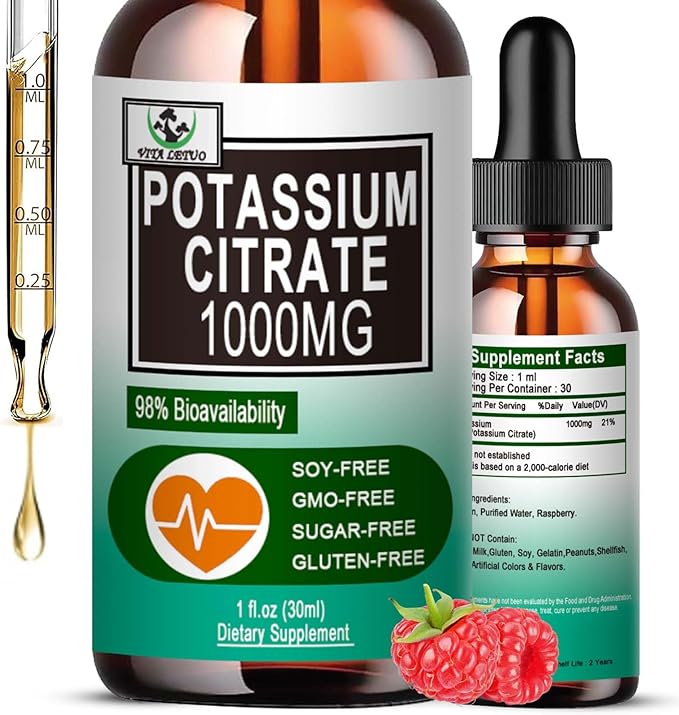
8- Potassium Supplements: Helpful or Harmful?
Supplements may seem like a shortcut, but they come with caveats. High doses of potassium in pill form can be dangerous, particularly for individuals with kidney disease or those on certain medications.
Dr. Walter Willett of Harvard’s T.H. Chan School of Public Health warns that “whole foods provide not just potassium, but a synergistic mix of nutrients that supplements can’t replicate.” Unless prescribed by a physician, potassium should ideally come from dietary sources.

9- Exercise and Potassium Synergy
Physical activity complements potassium intake by enhancing circulation, improving arterial flexibility, and increasing kidney efficiency in sodium excretion. Regular exercise and potassium intake act like a two-pronged approach to lowering blood pressure.
Even moderate aerobic exercise—30 minutes a day, five times a week—can amplify potassium’s effects. According to The American College of Sports Medicine, combining diet and exercise has a cumulative effect on blood pressure reduction and cardiovascular resilience.

10- Sodium Reduction Still Matters
While boosting potassium is critical, that doesn’t mean sodium should be ignored. The key is balance. Most Americans consume more than 3,400 mg of sodium daily, well above the recommended 2,300 mg. This overload disrupts fluid balance and strains blood vessels.
Cutting back on sodium-rich condiments, processed meats, and salty snacks remains a valuable strategy. But it should go hand-in-hand with potassium enhancement to fully address the hypertension epidemic.

11- The Renin-Angiotensin-Aldosterone System (RAAS)
Potassium affects blood pressure by interacting with the RAAS—a hormonal system that regulates fluid balance and blood vessel constriction. When potassium levels are sufficient, the RAAS is suppressed, leading to lower blood pressure.
This system is also the target of many blood pressure medications. Interestingly, nature provides its own modulation of RAAS through diet. As outlined in Human Physiology: From Cells to Systems by Lauralee Sherwood, dietary potassium is a natural ally in controlling this complex system.

12- Potassium and Kidney Health
Healthy kidneys are essential for maintaining mineral balance. Potassium helps them flush out excess sodium efficiently. In turn, well-functioning kidneys prevent hypertension-related damage to delicate blood vessels.
However, those with chronic kidney disease must manage potassium intake carefully. A healthcare provider can determine safe levels, ensuring that the benefits of potassium don’t become a burden to compromised renal systems.

13- Stress, Cortisol, and Mineral Imbalance
Chronic stress elevates cortisol, a hormone that disrupts mineral retention and blood pressure regulation. Potassium can help moderate this hormonal storm by supporting adrenal health and buffering sodium retention.
Mindfulness practices, combined with a potassium-rich diet, may provide a holistic way to address both psychological and physiological components of hypertension. As Dr. Dean Ornish notes, “What we eat, how we respond to stress, and how much love and support we have… all affect our health and longevity.”

14- Sleep Quality and Mineral Balance
Poor sleep has been linked to higher blood pressure. Sleep deprivation alters hormone levels and reduces the body’s ability to regulate sodium and potassium.
Ensuring adequate potassium intake supports cellular relaxation and may enhance sleep quality, creating a virtuous cycle. Why We Sleep by Dr. Matthew Walker emphasizes that nutrient intake and circadian rhythms are intricately linked—a fact often overlooked in hypertension management.

15- Potassium and Bone Health
Potassium doesn’t just support blood pressure—it also helps maintain bone density. It does so by buffering dietary acid load and reducing calcium loss through urine. A high-potassium diet has been linked to stronger bones and reduced fracture risk.
The dual benefit makes potassium an essential mineral for aging populations. According to The Nutritional Biochemistry of Potassium by Robert Heaney, diets rich in potassium correlate with better skeletal health, especially in postmenopausal women.

16- Tracking Intake: The Role of Food Journals
Keeping a food journal can help monitor potassium intake, revealing gaps and opportunities for improvement. Apps like Cronometer or MyFitnessPal allow users to track nutrient intake with precision.
This practice cultivates nutritional mindfulness. Awareness leads to change, and change leads to results. Journaling also helps identify food patterns that may contribute to high sodium intake or poor potassium absorption.

17- Educating Patients and Practitioners
Medical practitioners often focus on sodium but overlook potassium in dietary counseling. Educational initiatives should empower both doctors and patients to address this imbalance comprehensively.
Books like How Not to Die by Dr. Michael Greger advocate for dietary change as frontline therapy. Integrating nutritional education into routine care could transform hypertension treatment from reactive to proactive.

18- Community Health Initiatives
Public health campaigns can promote potassium-rich diets through school programs, media, and community gardens. Education must start early to instill lifelong habits.
Government partnerships with grocery stores and local farms can help bring affordable produce to underserved communities. As the WHO notes, “Population-wide sodium reduction and potassium enhancement is a global imperative for cardiovascular health.”

19- Culinary Techniques for Potassium Retention
Cooking methods affect potassium content. Boiling can leach potassium into water, while steaming, roasting, and sautéing preserve more of the mineral. Choosing the right preparation method ensures maximum benefit.
Culinary creativity also matters. Incorporating herbs, spices, citrus, and umami-rich ingredients can enhance flavor without relying on salt, making high-potassium meals both healthful and enjoyable.

20- Personalized Nutrition Plans
Not all bodies respond the same way to dietary changes. Genetics, gut microbiota, and pre-existing health conditions influence how potassium is metabolized. Personalized nutrition considers these variables.
Registered dietitians can help develop tailored plans that optimize mineral balance while respecting individual needs. Precision nutrition is the future—and potassium is a cornerstone of that vision.

21- Potassium vs. Sodium: A Paradigm Shift in Blood Pressure Management
Recent research underscores that increasing potassium intake may be more effective in lowering blood pressure than reducing sodium alone. While sodium reduction remains a cornerstone of hypertension treatment, the latest evidence suggests that bolstering potassium levels yields superior cardiovascular outcomes—especially in individuals with diets high in sodium.
In a groundbreaking study published in Hypertension, researchers found that diets rich in potassium lowered systolic pressure significantly more than diets focused exclusively on sodium restriction. This challenges the traditional dogma of salt elimination and invites a more holistic nutritional strategy: balance over avoidance.

22- How Potassium Supports Vascular and Renal Function
Potassium plays a dual role in regulating blood pressure. First, it relaxes blood vessels by reducing tension in the muscular walls of arteries. This vasodilation allows for smoother blood flow and less resistance. Second, it enhances kidney function by assisting in the elimination of excess sodium through urine.
As the American Journal of Clinical Nutrition explains, this one-two punch—relaxing blood vessels and aiding sodium excretion—makes potassium a powerful tool for managing hypertension. The mineral doesn’t just balance sodium; it actively helps the body purge its harmful excesses.

23- Everyday Foods That Deliver Potassium
You don’t need expensive supplements or exotic foods to meet your potassium needs. Everyday staples like bananas, lentils, potatoes, spinach, yogurt, and salmon are naturally high in this mineral. These options also offer secondary benefits such as fiber, antioxidants, and omega-3s.
Nutrition expert Dr. David Katz notes that “a balanced diet rich in whole, minimally processed foods will automatically be higher in potassium and lower in sodium.” This makes potassium intake a byproduct of good eating habits, not just a targeted intervention.

24- New Research Shows Potassium May Be Easier and More Effective
The emerging consensus from new studies suggests that adding potassium-rich foods may be both simpler and more effective than trying to eliminate all sources of sodium. This is especially valuable in a world where processed food is hard to avoid entirely.
In practical terms, this means shifting the dietary focus from restriction to inclusion. A study in The Lancet found that participants who focused on increasing potassium had better long-term adherence and outcomes than those told to avoid sodium-rich foods.

25- A Symbiotic Relationship: Sodium and Potassium Together
Rather than existing in opposition, sodium and potassium work together to regulate fluid balance, nerve signals, and blood pressure. The key lies in the ratio between the two. When potassium levels are high, it neutralizes sodium’s hypertensive effects.
Dr. Dariush Mozaffarian, dean at the Friedman School of Nutrition, summarizes it well: “It’s not just about cutting back on sodium—it’s about restoring the natural mineral balance that supports vascular health.”

26- Potassium-Rich Foods That Outperform Salt Cuts
Research shows that adding potassium-rich foods like bananas or broccoli to your diet can yield more measurable results than merely cutting back on salt. This is especially true for individuals who find it difficult to eliminate salty snacks entirely.
Including foods like Swiss chard, edamame, or avocados in meals provides a delicious and satisfying way to shift your mineral intake in favor of potassium, reducing dependence on rigid sodium control strategies.
27- What the New Research Says
Recent clinical trials and meta-analyses have turned the spotlight on potassium’s overlooked potential. One major review in BMJ Open concluded that potassium intake significantly reduced blood pressure in adults, independent of sodium levels.
This reflects a growing recognition that hypertension is a multifaceted issue, requiring more than just a reductionist approach to salt. Nutrition science now favors a broader, systems-based strategy—of which potassium is a vital part.

28- The Potassium-Sodium Ratio: A Crucial Metric
Rather than focusing solely on absolute intake, researchers now emphasize the ratio of potassium to sodium. A higher potassium-to-sodium ratio correlates with lower blood pressure and decreased cardiovascular risk.
In simple terms, even if you consume some sodium, balancing it with enough potassium mitigates its harmful effects. The World Health Organization recommends a dietary potassium-to-sodium ratio of at least 1:1—but higher is often better.

29- Potassium Lowers Blood Pressure, Even With Normal Sodium
One of the most compelling findings is that higher dietary potassium helps lower blood pressure regardless of sodium intake. Whether you eat a high- or normal-sodium diet, potassium still exerts a protective effect.
This discovery is vital for populations with limited access to low-sodium foods. As long as potassium intake is sufficient, the adverse impact of sodium can be partially buffered—offering a more flexible dietary path.

30- The Science Behind the Mineral Interaction
The interplay between sodium, potassium, and blood pressure is rooted in human physiology. Sodium draws water into the bloodstream, raising volume and pressure. Potassium counteracts this by encouraging the kidneys to release both water and sodium.
This homeostatic relationship ensures fluid equilibrium and vascular health. As described in Guyton and Hall Textbook of Medical Physiology, this mineral interaction is central to the body’s regulation of blood pressure and fluid balance.

31- Potassium Relaxes Blood Vessel Walls
Unlike sodium, which stiffens arterial walls, potassium acts as a natural relaxant. It improves endothelial function and reduces vascular resistance, making it easier for blood to flow and pressure to drop.
This property positions potassium as not just a balancing mineral, but a direct therapeutic agent. Its vasodilatory effect makes it invaluable in cardiovascular disease prevention and treatment.

32- Potassium and Kidney Synergy
Potassium’s action on the kidneys is crucial. It facilitates the removal of sodium by altering the renal sodium-potassium exchange mechanisms, thereby supporting blood pressure control at a systemic level.
This renal function is particularly beneficial in those with mild kidney impairment. However, those with advanced kidney disease should approach potassium intake cautiously and under medical supervision.

33- The Role of Kidney Transporters
Your kidneys rely on specialized proteins—sodium-potassium pumps and transporters—to excrete sodium effectively. These mechanisms depend on adequate potassium levels to function optimally.
Without enough potassium, sodium transport is inefficient, leading to its accumulation and subsequent hypertension. This is why diets low in potassium often fail to control blood pressure, even when sodium is limited.

34- Eat More Potassium, Retain Less Sodium
Simply put, increasing potassium intake leads to decreased sodium retention. This effect is both biochemical and clinical, resulting in lowered blood volume and less arterial strain.
It’s a principle backed by numerous peer-reviewed studies: for every gram of potassium consumed, the body excretes more sodium. This makes potassium intake a strategic lever in controlling high blood pressure.
35- Potassium-Rich Foods That Pack a Punch
Beyond bananas, a wide variety of foods are excellent sources of potassium. Baked potatoes, white beans, spinach, lentils, and salmon are among the top contributors. These foods also offer fiber, vitamins, and healthy fats.
Incorporating a mix of these items into your weekly meals not only ensures potassium adequacy but supports overall nutrition. Diverse sources also reduce monotony, helping to sustain long-term dietary changes.

36- Why Food Sources Beat Supplements
Potassium supplements may seem convenient, but they come with risks—especially for individuals with kidney issues or those taking certain medications. Moreover, food sources provide potassium in a more bioavailable, balanced form.
Whole foods contain additional nutrients like magnesium and fiber, which work synergistically to enhance cardiovascular health. Therefore, unless medically advised, food remains the safest and most effective way to meet potassium needs.

37- Understanding Recommended Daily Intake
The FDA has set the Daily Value (DV) for potassium at 4,700 milligrams. Meanwhile, the American Heart Association suggests a therapeutic range of 3,500 to 5,000 milligrams for individuals managing high blood pressure.
These benchmarks provide a target for dietary planning. Tracking intake through apps or food labels can help ensure you’re meeting this crucial health goal—without over-relying on supplements.

38- Gender-Specific Potassium Needs
Potassium needs vary by sex. Men should aim for at least 3,400 mg/day, while women require around 2,600 mg. This difference accounts for variations in muscle mass and metabolic rate.
Personalized nutrition acknowledges these distinctions. Tailoring potassium intake to individual needs—whether by sex, age, or health status—can maximize benefits while minimizing risks.

39- Beyond Bananas: Unsung Potassium Heroes
While bananas are widely recognized for their potassium content, they’re far from the only option. Apricots, lentils, baked potatoes, spinach, and salmon are equally potent—and often more versatile in meals.
Diversifying your potassium sources not only prevents palate fatigue but also enriches your diet with complementary nutrients. This variety is key to creating a sustainable and enjoyable eating plan.
40- Finding the Right Potassium-to-Sodium Ratio
There’s no universal golden ratio for potassium and sodium. Factors such as health conditions, physical activity, and dietary habits all influence the ideal balance.
Routhenstein, a leading clinical dietitian, recommends a personalized approach: “Work with your healthcare provider to determine the ratio that supports your unique physiology and lifestyle.”

41- Personalizing Your Ratio for Optimal Health
Given the complex interaction between diet and genetics, no one-size-fits-all ratio applies. What matters most is the direction—moving toward higher potassium and lower sodium.
Health professionals can help calibrate this based on lab results, dietary patterns, and risk factors. This personalized strategy offers better compliance and longer-lasting health benefits.

42- The Case for Lower Sodium Intake
The American Heart Association advises limiting daily sodium to between 1,500 and 2,300 mg. Staying within this range reduces the risk of hypertension, stroke, and kidney damage.
While this may seem restrictive, it’s achievable with mindful choices: preparing meals at home, using herbs instead of salt, and avoiding processed snacks can make a significant difference.
43- Small Tweaks, Big Results
Cutting sodium and increasing potassium doesn’t require an overhaul. Even modest changes—like swapping chips for nuts or soda for orange juice—can shift the mineral balance significantly.
Consistency is more important than perfection. Over time, small daily improvements build a powerful shield against high blood pressure and cardiovascular disease.

44- Cap Sodium at 2,300 mg Daily
Setting a firm upper limit of 2,300 mg of sodium per day is a key benchmark. Achieving this requires label-reading, awareness, and often cooking more at home.
Salt isn’t just in obvious items—it’s hidden in breads, condiments, and sauces. Awareness is the first step toward sodium reduction and better heart health.

45- Ease Into Potassium
While potassium is beneficial, sudden increases can cause digestive discomfort or imbalances in those with kidney conditions. Gradual increments are safer and more sustainable.
Start by adding one high-potassium food per day. As your palate and body adjust, gradually build up toward your daily goal—without overwhelming your system.
46- One Swap Per Meal
An easy strategy is to make one potassium-rich swap at every meal. Add avocado to toast, replace chips with sweet potato, or enjoy a side of lentils instead of rice.
This practical tip aligns with behavioral psychology: incremental changes are easier to adopt and stick with long-term, promoting better adherence and outcomes.

47- Enjoyable Diets Are Sustainable Diets
Taste matters. If your diet isn’t enjoyable, it won’t be sustainable. Incorporate foods you love that also happen to be high in potassium—whether that’s mango, coconut water, or roasted vegetables.
Health isn’t just about nutrients—it’s about lifestyle. A pleasurable diet is a diet that lasts, bringing both joy and wellness to the table.

48- Go Slow to Go Far
Trying to overhaul your entire diet overnight often backfires. A gradual, thoughtful approach increases the chances of long-term success. Allow yourself time to adapt, explore, and enjoy the process.
As with any lifestyle change, patience is key. Think of potassium-rich eating not as a crash diet, but as a lifelong journey toward better health.

49- Reiterate: Food Over Supplements
Potassium supplements, while sometimes necessary, carry safety concerns like gastrointestinal distress and arrhythmias. Whole foods provide a safer and more nourishing option.
Unless advised by a healthcare provider, prioritize food as your potassium source. The body processes it more efficiently, and you gain the added benefits of fiber, antioxidants, and satiety.

50- Final Word: More Potassium, Lower Pressure
The science is clear: more dietary potassium leads to lower blood pressure—even in the context of varying sodium intakes. This effect is consistent, measurable, and sustainable.
Incorporating potassium-rich foods into your daily routine isn’t just a nutritional upgrade—it’s a preventive health strategy. One that could add years to your life and life to your years.
Conclusion
In the battle against high blood pressure, the silent champion may not be what you remove—but what you add. Potassium-rich foods, often overlooked, wield profound power in restoring cardiovascular balance. From cellular mechanics to public health implications, the evidence is compelling: potassium deserves a central role in our dietary strategy.
Rather than demonizing sodium in isolation, a more nuanced approach calls for nutritional harmony. As we’ve seen, boosting potassium not only counteracts the adverse effects of sodium but also supports kidney function, vascular health, and overall wellbeing. Let’s rewrite the hypertension playbook with potassium at its heart—because prevention starts on our plates.

Focusing solely on reducing sodium is like addressing only one side of an equation. To truly tackle high blood pressure, we must embrace potassium as a co-equal partner in cardiovascular health. From leafy greens to legumes, from policy reform to personal food choices, the path forward lies in restoring our body’s natural mineral harmony.
As Hippocrates wisely said, “Let food be thy medicine.” In the realm of hypertension, potassium is one of the most powerful prescriptions nature has to offer. Let’s not leave it off the table.

Bibliography
- Appel, Lawrence J., et al. Effects of Comprehensive Lifestyle Modification on Blood Pressure Control: Main Results of the PREMIER Clinical Trial. JAMA, 2003.
— A landmark study showing the combined effects of dietary change, physical activity, and behavioral modification on blood pressure. - Whelton, Paul K., et al. Sodium, Potassium, and Blood Pressure: Emerging Evidence for More Potassium, Less Sodium. The New England Journal of Medicine, 1997.
— Discusses the interplay between sodium and potassium and how they affect blood pressure regulation. - He, Feng J., and MacGregor, Graham A. Beneficial Effects of Potassium on Human Health. Physiologia Plantarum, 2008.
— A detailed overview of potassium’s physiological benefits and its role in disease prevention. - Heller, Marla. The DASH Diet Action Plan. Hachette Books, 2007.
— Practical guide based on the DASH diet, emphasizing the role of potassium-rich foods in managing hypertension. - Sherwood, Lauralee. Human Physiology: From Cells to Systems. Cengage Learning, 2015.
— An authoritative textbook covering the physiological mechanisms of electrolyte balance and blood pressure regulation. - Greger, Michael. How Not to Die: Discover the Foods Scientifically Proven to Prevent and Reverse Disease. Flatiron Books, 2015.
— Advocates plant-based, potassium-rich diets for longevity and prevention of chronic illnesses including hypertension. - Mozaffarian, Dariush. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation, 2016.
— Offers insights into how dietary patterns affect cardiovascular outcomes, emphasizing potassium’s protective role. - Walker, Matthew. Why We Sleep: Unlocking the Power of Sleep and Dreams. Scribner, 2017.
— Connects nutrient intake, including potassium, with sleep quality and blood pressure regulation. - Nestle, Marion. What to Eat. North Point Press, 2006.
— Offers practical nutritional advice and explains the health impact of mineral intake, including sodium and potassium. - Pollan, Michael. In Defense of Food: An Eater’s Manifesto. Penguin Press, 2008.
— Advocates for a whole-food diet rich in vegetables and legumes that are naturally high in potassium. - Heaney, Robert P. The Nutritional Biochemistry of Potassium. In Calcium and Phosphorus in Health and Disease, CRC Press, 2000.
— Discusses how potassium contributes to bone health and interacts with other minerals. - Fuhrman, Joel. Eat to Live: The Amazing Nutrient-Rich Program for Fast and Sustained Weight Loss. Little, Brown and Company, 2011.
— Emphasizes the power of legumes and leafy greens—high in potassium—for metabolic and cardiovascular health. - Guyton, Arthur C., and Hall, John E. Textbook of Medical Physiology. Elsevier, 13th ed., 2015.
— A comprehensive reference on kidney physiology and mineral balance relevant to blood pressure. - World Health Organization (WHO). Guideline: Sodium Intake for Adults and Children. Geneva, 2012.
— Sets global recommendations for sodium and potassium intake to reduce cardiovascular disease burden. - American Heart Association. Sodium and Potassium: How They Affect Your Heart Health. AHA Publications, 2021.
— Educational material providing practical guidelines for managing blood pressure through dietary changes. - Katz, David L., and Meller, Sonja. Can We Say What Diet Is Best for Health?. Annual Review of Public Health, 2014.
— Reviews evidence on dietary patterns and the role of potassium in promoting health. - Routhenstein, Nicole. Clinical Dietitian, quoted in various interviews and publications on the potassium-to-sodium ratio and personalized nutrition strategies.
— Provides expert insight into dietary customization and mineral balance. - Ornish, Dean. The Spectrum: A Scientifically Proven Program to Feel Better, Live Longer, Lose Weight, and Gain Health. Ballantine Books, 2008.
— Advocates for lifestyle medicine with an emphasis on plant-based, high-potassium foods. - Katz, David L. Nutrition in Clinical Practice: A Comprehensive, Evidence-Based Manual for the Practitioner. Lippincott Williams & Wilkins, 2012.
— Offers in-depth analysis of clinical nutrition strategies including potassium management in hypertensive patients. - Hypertension. Potassium Intake and Blood Pressure: A Meta-Analysis of Randomized Controlled Trials. American Heart Association Journal, 2005.
— Summarizes findings across multiple studies confirming the positive effect of potassium on blood pressure.

By Amjad Izhar
Contact: amjad.izhar@gmail.com
https://amjadizhar.blog
Affiliate Disclosure: This blog may contain affiliate links, which means I may earn a small commission if you click on the link and make a purchase. This comes at no additional cost to you. I only recommend products or services that I believe will add value to my readers. Your support helps keep this blog running and allows me to continue providing you with quality content. Thank you for your support!




